Health
Understanding Menopause Joint Pain: Causes, Symptoms, and Management Strategies
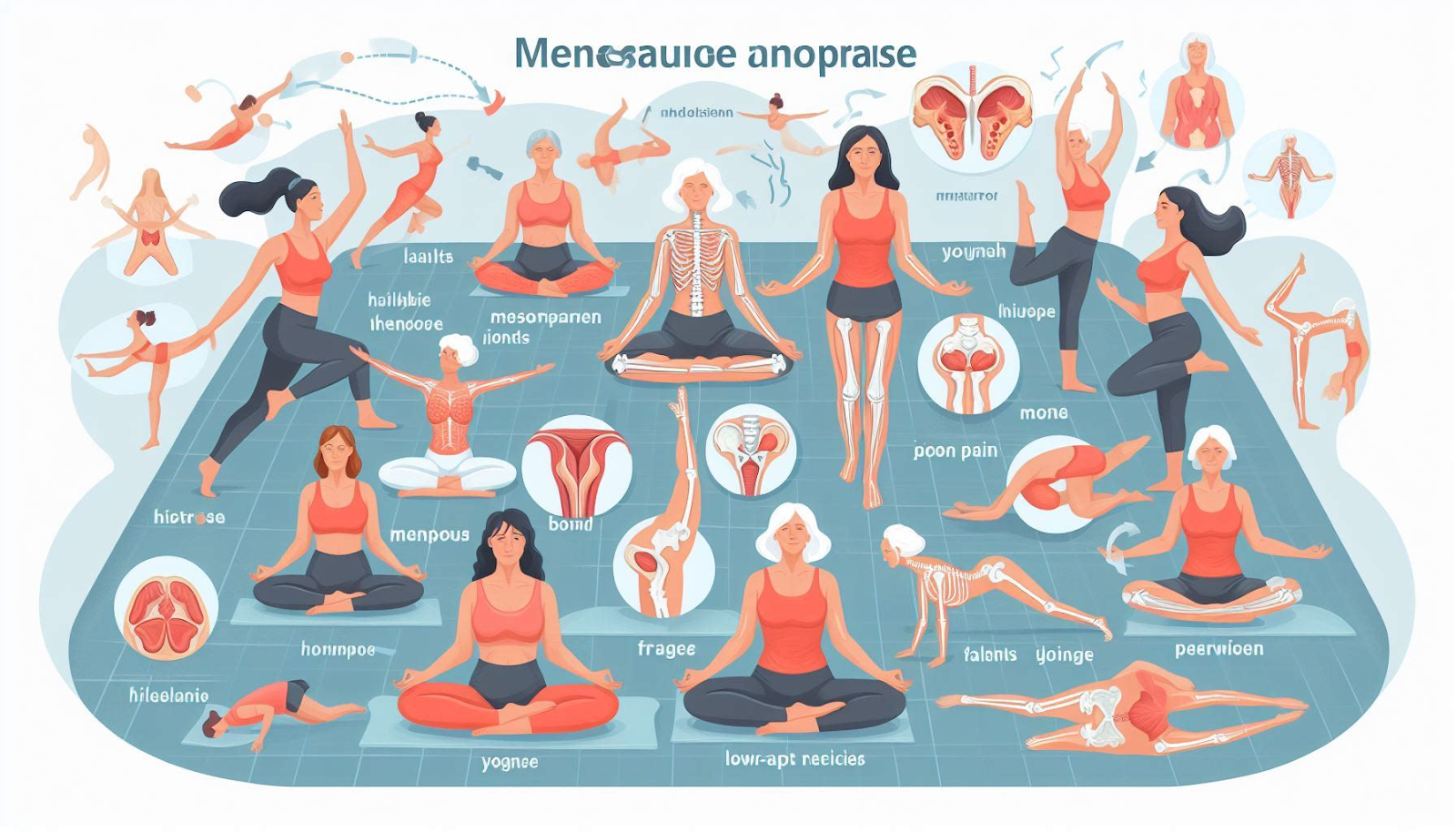
For many women, the transition to menopause brings a host of challenging symptoms, from hot flashes and mood changes to sleep disturbances and weight fluctuations. However, one often overlooked aspect of this life stage is the increased risk of joint pain and discomfort. As hormonal shifts occur during menopause, the likelihood of developing musculoskeletal issues such as osteoarthritis and rheumatoid arthritis rises, making it crucial for women to understand the underlying causes, recognize the symptoms, and explore effective management strategies.
Causes of Menopausal Joint Pain
The primary culprit behind joint pain during menopause is the fluctuation and eventual decline in estrogen levels. Estrogen plays a vital role in maintaining healthy joints and bones, and its depletion can lead to several physiological changes that contribute to joint discomfort.
1. Bone Loss: Estrogen helps to regulate bone metabolism and maintain bone density. When estrogen levels drop during menopause, the rate of bone loss accelerates, increasing the risk of osteoporosis. This weakening of bones can make joints more susceptible to injury and inflammation, leading to pain and stiffness.
2. Cartilage Degeneration: Estrogen also plays a role in the health and maintenance of cartilage, the smooth connective tissue that cushions the joints. As estrogen levels decline, the cartilage may become thinner and more susceptible to wear and tear, leading to joint pain and decreased mobility.
3. Inflammation: Estrogen has anti-inflammatory properties, and its deficiency during menopause can contribute to increased inflammation in the body. This inflammation can affect the joints, causing swelling, stiffness, and pain.
4. Autoimmune Disorders: Women are more susceptible to developing autoimmune disorders like rheumatoid arthritis during and after menopause. These conditions can cause joint pain, swelling, and deformity due to the body’s immune system attacking its own healthy tissues.
Symptoms of Menopausal Joint Pain
The symptoms of joint pain during menopause can vary in severity and location, but some common manifestations include:
1. Joint Stiffness: Women may experience stiffness in their joints, particularly in the morning or after periods of inactivity. This stiffness can make it challenging to perform daily activities and may be accompanied by a decreased range of motion.
2. Joint Swelling: Inflammation in the joints can lead to swelling, which may be more noticeable in the hands, knees, and feet.
3. Joint Pain: Pain in the joints is a common complaint during menopause, affecting areas such as the hips, knees, ankles, and hands. The pain may be dull, aching, or sharp, and can worsen with movement or weight-bearing activities.
4. Muscle Weakness: As joint pain and stiffness increase, women may experience muscle weakness, making it difficult to perform everyday tasks or engage in physical activities.
5. Reduced Mobility: In severe cases, joint pain and stiffness can significantly limit mobility, making it challenging to walk, climb stairs, or perform other activities.
Management Strategies for Menopausal Joint Pain
While joint pain during menopause can be debilitating, there are various management strategies that women can employ to alleviate their symptoms and improve their quality of life.
1. Hormone Therapy: For women experiencing severe menopausal symptoms, including joint pain, hormone therapy (HT) may be recommended. HT involves the administration of estrogen, either alone or in combination with progesterone, to help alleviate menopausal symptoms by restoring hormonal balance. However, HT should be carefully considered and discussed with a healthcare provider, as it may have potential risks and side effects.
2. Pain Medication: Over-the-counter pain medications, such as acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs), can provide temporary relief from joint pain and inflammation. However, it’s important to consult with a healthcare provider before taking any medication, as some may have side effects or interact with other medications.
3. Exercise and Physical Therapy: Engaging in low-impact exercises, such as swimming, cycling, or strength training, can help to improve joint flexibility, strengthen surrounding muscles, and reduce pain. Physical therapy can also be beneficial, as a trained therapist can design an exercise program tailored to an individual’s needs and limitations.
4. Weight Management: Maintaining a healthy weight can help to reduce the stress on weight-bearing joints, such as the knees and hips. A balanced diet and regular exercise can aid in weight management and may alleviate joint pain.
5. Lifestyle Modifications: Making simple lifestyle changes can also help manage joint pain during menopause. These may include using assistive devices (like canes or braces) to reduce joint stress, practicing stress-reducing techniques (like yoga or meditation), and ensuring adequate rest and sleep.
6. Alternative Therapies: Many women find relief through alternative therapies, such as acupuncture, massage therapy, or dietary supplements like glucosamine and chondroitin sulfate. However, it’s essential to consult with a healthcare provider before trying any alternative therapies, as some may have potential side effects or interact with medications.
7. Joint Surgery: In severe cases, where joint pain and disability significantly impact quality of life, joint replacement surgery may be recommended. However, this is typically a last resort for individuals who have not found relief through other management strategies.
Coping with joint pain during menopause can be challenging, but by understanding the underlying causes, recognizing the symptoms, and exploring various management strategies, women can take an active role in alleviating their discomfort and maintaining their overall well-being.
It’s important to remember that every woman’s experience with menopause and joint pain is unique, and what works for one individual may not work for another. Open communication with a healthcare provider is crucial to developing an effective management plan tailored to individual needs and circumstances.
By embracing a proactive approach and seeking support when needed, women can navigate the menopausal transition with greater confidence and comfort, minimizing the impact of joint pain on their daily lives and overall quality of life.
