Health
Does Obesity Posses Higher Risk Of Diabetes? Addressing the Impact of Obesity

Obesity and diabetes represent two significant global public health crises that are closely interrelated. Obesity increases the risk of developing type 2 diabetes. With rising obesity rates worldwide, diabetes prevalence has also climbed dramatically.
This article explores the link between obesity and diabetes, the mechanisms behind the connection, complications that can arise, and preventive lifestyle measures and medical interventions to reduce diabetes risk.
Understanding Diabetes
Diabetes involves abnormal blood sugar regulation stemming from inadequate insulin secretion by the pancreas or improper insulin utilization in the body’s cells. Type 1 diabetes results from autoimmune destruction of insulin-producing beta cells. Type 2 diabetes arises from progressive insulin resistance coupled with defective insulin secretion. Gestational diabetes occurs during pregnancy.
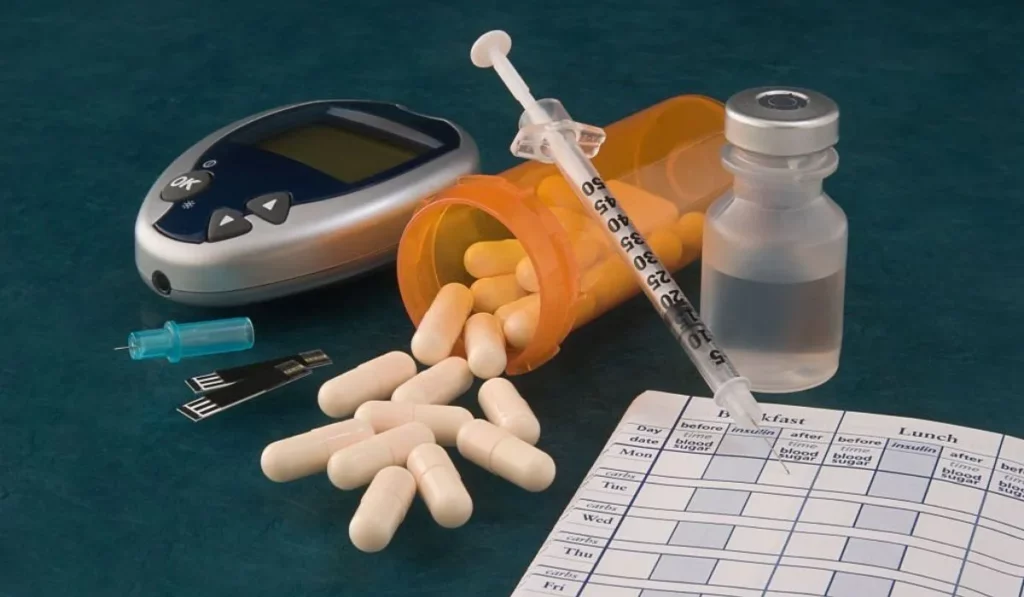
Without sufficient insulin or insulin sensitivity, blood glucose levels become elevated, leading to complications like nerve damage, kidney disease, vision loss, and cardiovascular disease if uncontrolled.
The Obesity Epidemic
Global obesity rates have nearly tripled since 1975. The primary drivers are increased calorie consumption, sedentary lifestyles, and constant access to processed high-calorie foods. Genetics, medical conditions, socioeconomic factors, and obesity-promoting environments also contribute.
Obesity is associated with many other health risks including heart disease, stroke, high blood pressure, cancers, respiratory issues, fatty liver disease, kidney disease, osteoarthritis, and reduced life expectancy. Tackling obesity is imperative for public health.
Linking Obesity and Diabetes
Obesity significantly increases the risk of developing type 2 diabetes. Excess weight, especially abdominal fat, alters hormone and cytokine signaling, creating a chronic inflammatory state and insulin resistance. Fat cells release fatty acids, resistin, and other molecules that impair glucose uptake and insulin signaling.
Obesity also stresses pancreatic beta cells to produce more insulin initially, leading to exhaustion and burnout over time. Just a modest weight loss of 5-10% in obese individuals can sharply reduce diabetes risk by restoring insulin sensitivity and beta cell function.
Mechanisms Behind The Connection
There are several mechanisms by which obesity induces insulin resistance and diabetes progression. Excess fatty acids released from enlarged fat cells reduce insulin signaling. Adipocytes secrete more hormones like resist in and cytokines like TNF-alpha that both impede insulin action.
Obesity creates inflammation mediated by immune cells within fat tissue that alters insulin pathway functioning. Obese individuals exhibit mitochondrial dysfunction and impaired adipocyte differentiation that negatively impact glucose metabolism. Visceral abdominal fat appears most metabolically active in driving insulin resistance through these pathways.
Obesity And Type 2 Diabetes Risk Factors
Genetics influence both obesity and diabetes risk, but lifestyle factors play a major role. Sedentary behavior coupled with excessive calorie intake from highly processed foods fosters weight gain and metabolic dysfunction. Stress, low socioeconomic status, and limited health knowledge promote such behaviors.
Unhealthy diets high in saturated fats, sugars, and refined carbohydrates also provoke obesity and impaired glucose metabolism. Family history, ethnicity, increasing age, and female gender correlate with higher risks. Identifying and mitigating modifiable risk factors through education and lifestyle interventions is crucial.
The Role of Body Mass Index (BMI)
Body mass index (BMI) estimates body fat percentage using height and weight measurements. Online calculators classify BMI into underweight, normal, overweight, obese, and morbidly obese categories. A BMI exceeding 25 kg/m2 indicates overweight. Obesity is defined by a BMI of 30 kg/m2 or higher. Severe obesity occurs at a BMI over 40 kg/m2.
Higher BMIs strongly predict type 2 diabetes risk as excessive weight strains the metabolic system. However, BMI has limitations in accuracy. Waist circumference and waist-hip ratio better estimate abdominal obesity driving insulin resistance. Body composition testing is also more precise.
Obesity-Related Health Complications
Obesity provokes numerous secondary health issues that compound diabetes severity and progression. Excess weight strains the cardiovascular system, increasing hypertension risk, which then accelerates diabetes complications.
Fatty liver disease, cholesterol abnormalities, sleep apnea, and lung conditions often accompany obesity and diabetes, increasing morbidity. Joint degradation from extra weight burden reduces mobility in diabetes patients. Managing obesity-related health risks improves diabetes outcomes. Even small amounts of weight loss can ease complications.
Read More:- How Does Diabetes Impact Sleep? Everything You Need To Know
Childhood Obesity and Early-Onset Diabetes
With childhood obesity rates tripling since the 1970s, type 2 diabetes is rising in youth. Obese children often become obese adults, priming insulin resistance progression at younger ages. Cardiometabolic abnormalities like hypertension, fatty liver, and dyslipidemia seen in obese youth advance diabetes development.
Lifestyle modifications to boost nutrition, and physical activity, and reduce sedentary time helps lower BMI and subsequent diabetes risks. Public health initiatives focused on preventing childhood obesity are critical to curtailing escalating youth type 2 diabetes rates.
Preventive Measures and Lifestyle Interventions
Regular physical activity, stress management, adequate sleep, and balanced nutrition with minimally processed foods supports diabetes prevention, especially with weight loss in overweight individuals.
Losing just 5-10% of body weight and keeping it off through calorie reduction and exercise markedly improves insulin sensitivity and diabetes risk factors. Structured lifestyle coaching and support groups boost success. Population-level policies targeting nutrition education, accessible recreation facilities, advertising regulations, and health-promoting food environments facilitate obesity and diabetes prevention.
Read More:- Foods To Avoid If You Have Diabetes -Say No To These Foods If You Have Diabetes!
Conclusion
In summary, extensive evidence demonstrates that obesity significantly escalates the risk of developing type 2 diabetes. Even modest sustained weight loss can dramatically lower diabetes risk among obese individuals. Complications of obesity further exacerbate diabetes severity and progression.
Addressing the global obesity epidemic through multi-level interventions is crucial for reducing diabetes prevalence worldwide.
